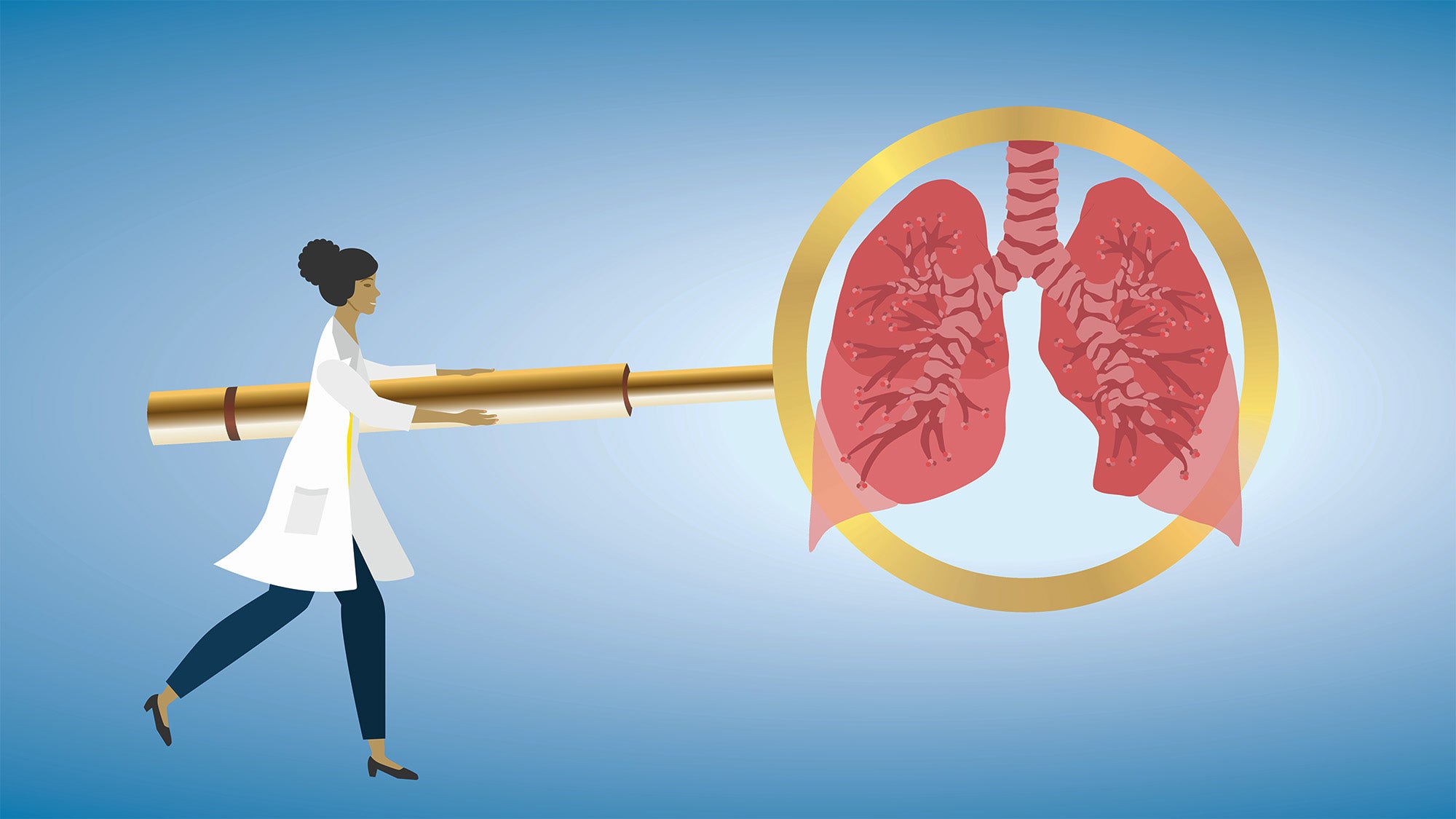
Georgetown Lombardi Faculty Members Aim To Improve Lung Cancer Screening and Smoking Cessation Rates by Focusing on Equity in Care
Posted in Lombardi Stories | Tagged cancer, cancer screening, early detection, health disparities, health equity, lung cancer, lung cancer screening, racial disparities, smoking cessation, tobacco control, underserved populations
(January 12, 2024) — As a behavioral scientist studying cancer, Kathryn Taylor, PhD, professor of oncology, chose to home in on evidence-based strategies to help reduce cancer-related mortality due to tobacco use. The work she co-leads with Randi Williams, PhD, assistant professor of oncology, as part of the Lung Screening, Tobacco, and Health (LSTH) research lab at Georgetown University’s Lombardi Comprehensive Cancer Center is especially relevant to underserved communities, who are often the target of tobacco product marketing.

At the heart of Taylor’s and Williams’ work is advancing promising early detection strategies and promoting proven smoking cessation efforts. Williams brings her background in public health and a lens of health equity to the LSTH lab, which is part of the Cancer Prevention & Control (CPC) Program at Georgetown Lombardi. Their work aligns with the goals set forth by the National Cancer Institute (NCI) and the Cancer Moonshot initiatives.
Their multipronged approach examines barriers of care that underserved populations face involving lung cancer screening referrals, smoking cessation referrals and treatment. Examples of different prongs include leveraging electronic health records to encourage more equitable promotion of lung cancer screenings and evaluating the effectiveness of using such screenings as an opportunity to encourage smoking cessation.
“We became interested in studying teachable moments associated with lung cancer screening among patients who smoke about 10 years ago,” said Taylor. “We see all of these areas fitting together: tobacco use assessment, tobacco treatment and lung cancer screenings.”
Increasing Referrals
The LSTH lab is currently running several research projects putting their approach into action, and they’re doing much of the work in collaboration with clinicians at MedStar Health, Georgetown’s academic health system partner.
“We take a multilevel view of determinants of tobacco-related disparities, including lung cancer, because we know we have to intervene at all levels in order to advance equity,” added Williams. “First, patients have to be identified for lung screening and cessation programs, which is why we are doing work with electronic health care records.”
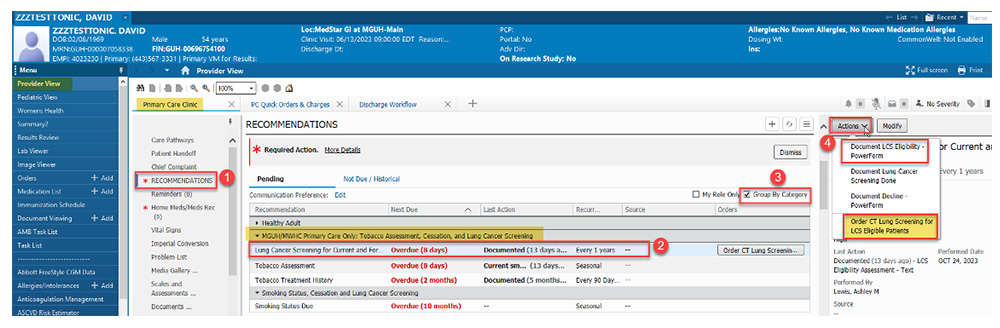
The DC Department of Health has funded a project with LSTH and MedStar Health that aims to modify electronic health records in how tobacco use is assessed to increase smoking cessation treatment referrals and lung cancer screening rates. Now providers receive an electronic message when accessing a patient’s record to consider a lung cancer screening referral for someone with a history of tobacco use. Taylor is currently tracking data to see if patient care is improved through the use of this modification.
“Medical records provide a way to target health systems to effect systemic change by having providers prompted for a referral for all eligible patients,” said Taylor.
Understanding Barriers to Screening
Williams is also taking the lead on a project funded by the NCI to address disparities between African American and white patients in lung cancer screening awareness.
“Our next prong is addressing barriers to screening in the clinical context between providers and patients,” said Williams. “We know there are barriers in health care systems that prevent lung cancer screening referrals for patients, especially Black patients, who are less likely to be referred for cancer screening and smoking cessation programs.”
“We’re working with four MedStar community-based primary care practices where the provider will receive a message that a patient is eligible for lung screening,” she added. “The patients that were identified will also receive outreach and education from our team about screenings.”
After both the provider and patient receive additional information, Williams is interested in investigating what happens in the clinical encounter and if the increased communication results in higher lung cancer screening rates.
“Does the provider place the order? Does the patient get screened for lung cancer?” she asked. “It’s important to remember that smoking is still highly stigmatized, and that stigma sometimes prevents patients from being open and honest in conversations with providers about their smoking history, which can result in a barrier to care.”
Smoking Cessation Projects
Another project directly relates to Taylor’s background as a clinical psychologist that began with funding from the NCI and is now funded by MedStar Health. The Smoking Treatment and Recovery (STAR) program, which began in 2018, seeks to encourage hematology and oncology patients at MedStar Washington Hospital Center and MedStar Georgetown University Hospital to quit smoking by participating in up to six phone-based counseling sessions with trained tobacco treatment specialists and nurse practitioners.

Breast cancer survivor Carolyn Wesley recounted receiving a phone call from a representative of the STAR program, who asked if she would be interested in joining. “I had been diagnosed with breast cancer the year before, and that was my reason to stop smoking,” said Wesley, who agreed to be part of STAR and was able to quit smoking.
“We found that the counseling sessions produce a 25% quit rate within six months of completing the sessions,” said Taylor, who has been tracking data from the project since it was launched in 2018.
The Tobacco Education and Lung Health (TEAL) project, funded by the NCI, takes a similar approach to STAR in investigating the effectiveness of smoking cessation telephone counseling with patients at high risk for lung cancer.
Taylor’s previous NCI trial found that offering intensive weekly smoking cessation counseling along with nicotine replacement resulted in a twofold greater cigarette quit rate compared to people who received minimal counseling and nicotine replacement. Patient participants were either enrolled in the “intensive” model of eight 20-minute sessions and eight weeks of nicotine patches or the “minimal” model of three counseling sessions and two weeks of patches.
“TEAL is expanding on this previous trial by addressing barriers to reach among underserved groups, who are less likely to receive cessation treatment,” said Williams. Another major goal of the new project is to understand what interventions are the most cost effective.
Whether it’s increasing the number of referrals for lung cancer screening or enrolling more oncology patients in smoking cessation programs, Taylor and Williams continue pursuing ways to improve lung cancer outcomes, especially for those who face the most barriers to care. Soon, Williams will begin a new study focused on developing methods of identifying people living with HIV who may benefit from lung cancer screening, sponsored by the DC Center for AIDS Research.
“Unfortunately, a lot of the disparities that exist outside of health care settings enter our health care systems, and we are interested in addressing systemic barriers to ensure more equitable cancer prevention and control care,” said Williams.
Heather Wilpone-Welborn
GUMC Communications