First-of-Its-Kind Clinical Trial at Georgetown Puts Mammography Technologies Under the Spotlight

Posted in Lombardi Stories | Tagged 3D mammography, breast cancer, cancer, cancer research, mammography
(July 31, 2020) — In the field of breast screening, 3D imaging, or tomosynthesis mammography, has become the go-to screening modality over conventional digital mammography in recent years.
But does 3D screening actually improve detection of — and survival from — life-threatening breast cancers, or does conventional mammography perform just as well at a lower cost?
Seeking to answer this very question, Georgetown Lombardi Comprehensive Cancer Center researchers are enrolling patients into a large-scale, randomized clinical trial with clinical partner MedStar Georgetown University Hospital, the only study site in the DC region. The Tomosynthesis Mammographic Imaging Screening Trial (TMIST) aims to enroll 165,000 patients in 100 sites in the U.S., with a few sites in Canada and Argentina.
Scientific Due Diligence
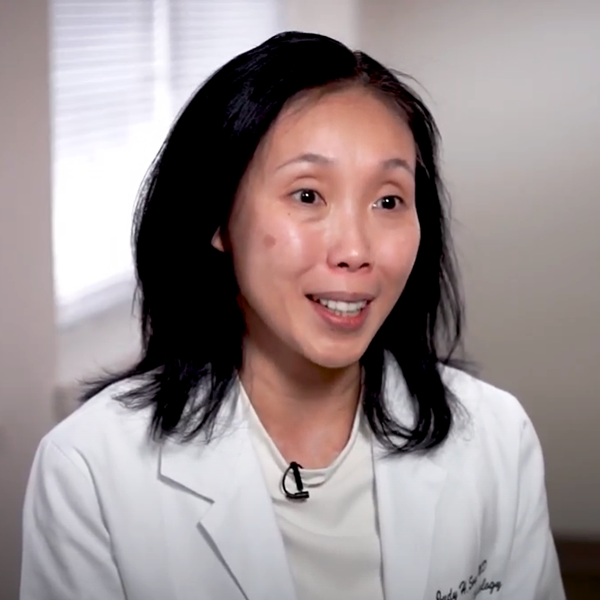
According to the study’s principal investigator, Judy Song, MD, chief of breast imaging at MedStar Georgetown and assistant professor of radiology at Georgetown University School of Medicine, this trial is a critical benchmark, in that it is the first time the two technologies will be compared in such a scientifically rigorous way.
She described this trial as “scientific due diligence,” similar to how the Digital Mammography Screening Trial — a randomized prospective study involving nearly 50,000 participants — compared digital to screen film mammography nearly two decades ago.
“Now we are now doing the legwork for 3D mammography, performing a similarly rigorous trial to validate the decision to implement it so broadly,” Song said.
While 3D mammography is widely used and highly touted for its higher sensitivity, the scientific community does not have the evidence to support if it is better at detecting tumor types known to be difficult to treat — including triple-negative and HER-positive tumors, or those that are larger or have spread to the lymph nodes — and whether it helps save lives.
TMIST seeks to determine if 3D technology leads to better outcomes for patients by unpacking the benefits and potential harms, such as callbacks for second mammograms, an increase in biopsies, or treatment that may not be necessary for tumors that are not aggressive or life-threatening.
At the core of this inquiry is the pursuit of precision medicine, according to Song. Particularly given the potentially higher cost of 3D mammography, it is valuable to understand the circumstances in which it is most warranted and beneficial.
“We hope this study will enable us to be even more thoughtful about how we are treating patients — it gets down to precision medicine,” she said. “We need to be conscious that there is no ‘one-size-fits-all’ approach when it comes to breast cancer.”
‘A Study for All People’
Researchers anticipate the trial may benefit minority populations, who statistically are less likely to enroll in clinical trials.

“This is the first study that really enables us to reach out and get a diverse group of people in terms of who participates in clinical trials,” said Lucile Adams-Campbell, PhD, who serves as the trial’s subinvestigator. “It is a study for all people — if you need a mammogram, you qualify.”
Adams-Campbell, a professor of oncology and associate director for minority health and health disparities research at Georgetown Lombardi, was the first patient to enroll in the trial at MedStar Georgetown.
“I’ve had over 30 years of mammograms, and almost all of them have been done in 2D, up until a few years ago when 3D came to Georgetown. So for me, it doesn’t matter which arm [of the study] I am in,” she said. “I think it’s important for women in the area to know that this is something available to all of us.”
Unprecedented Opportunity
Worta McCaskill-Stevens (M’85), MD, a nationally renowned medical oncologist and chief of the Community Oncology and Prevention Trials Research Group at the National Cancer Institute (NCI), was the second person to enroll.

Part of the team that designed TMIST, McCaskill-Stevens believes such a study represents an unprecedented opportunity for women of all races, ethnicities and backgrounds to take a more active role in thinking about their own screening and the implications of using one technology over another.
“Typically women, and particularly women of color, do not think much about clinical trials and screening. You get your appointment, go in, undress, get your film, and leave,” she said. “But it’s so important for us to engage all women in thinking about the fact that there are still outstanding research questions related to screening — ones that they can help answer.”
As part of her role at NCI, McCaskill-Stevens also directs the Community Oncology Research Program (NCORP), a nationwide network that seeks to bring cancer clinical trials and studies to underserved communities. Last August, Georgetown Lombardi was selected to establish the National Capital Area (NCA) NCORP through a $5.33 million grant under Adams-Campbell’s leadership.
One of the NCA-NCORP-established elements is Georgetown Lombardi’s Capital Breast Care Center (CBCC), which navigates primarily underserved, underinsured and uninsured women to receive mammography screening. Adams-Campbell said TMIST offers an important new screening opportunity for CBCC patients who choose to enroll.
A Moment to Reassess
The COVID-19 pandemic, which has already forced hospitals and clinics to reexamine basic decision-making and prioritization, including which procedures are essential and which can wait, also presents a unique moment to reassess standard protocols across the board.
“This is an opportunity to be more intentional in how we are treating patients — the pendulum is swinging,” Song said.
“There is now rapid commercialization of new technologies to market, and it is important for them to be put through rigorous scientific checks and balances. As clinicians, we must look at each patient and use the tools that will most benefit his or her care.”
For more information, please contact the Capital Breast Care Center at 202-784-2700.
Lauren Wolkoff (G’13)
GUMC Communications
