Biological Pathways Found That Drive Genomic Changes and Bone Metastasis in Ewing Sarcoma, a Rare Childhood Cancer
Posted in News Release | Tagged cancer, cancer research, Ewing sarcoma
Media Contact
Karen Teber
km463@georgetown.edu
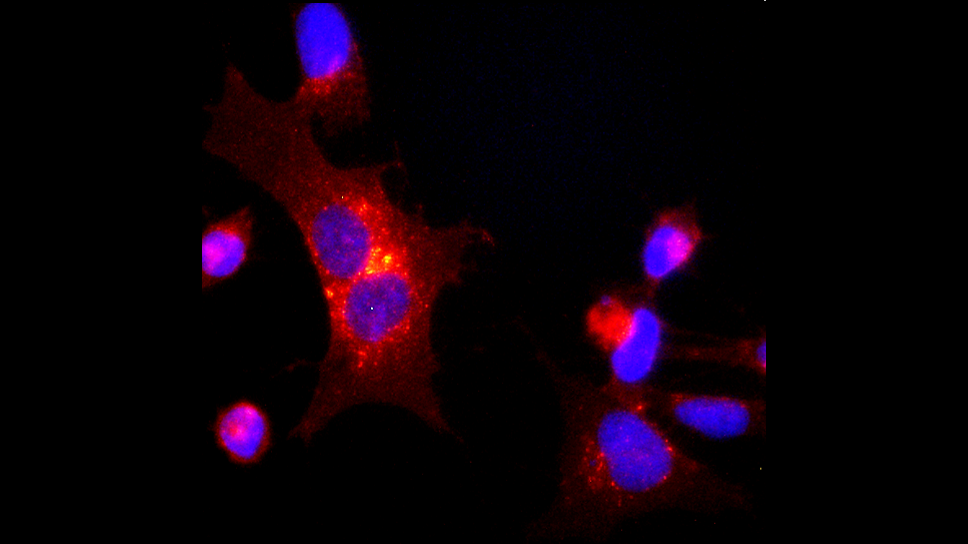
WASHINGTON (April 28, 2022) — In studies using mice grafted with human Ewing sarcoma tissue, researchers from Georgetown University Medical Center and colleagues have identified a biological pathway that is activated when tissue is starved of oxygen due to rapid growth of a tumor, thereby allowing cancer cells to make genetic changes so they can metastasize to the bone and thrive even when exposed to chemotherapy.
The pathway the scientists identified involves a receptor on the surface of a cancer cell, called Y5R, which plays a role in mediating oxygen-deprivation effects — if it was blocked or turned off, genetic changes would be limited, thereby inhibiting metastasis of a tumor.
The finding appeared April 28, 2022, in Nature Communications.
Each year, about 200 children and young adults in the United States are diagnosed with a Ewing tumor. About half of all Ewing sarcoma diagnoses are in people between the ages of 10 and 20; almost all cases of Ewing sarcoma occur in white and Hispanic people. If the tumor has spread to distant areas at the time of diagnosis, the 5-year survival rate is 38 percent but if it spreads to the bone, survival drops to between 8 and 14 percent.
“While the role of rapid genetic changes in spurring the growth of cancer is well known, the mechanisms initiating these changes are not well understood, and strategies to prevent them are lacking,” says Joanna Kitlinska, PhD, an associate professor in the Department of Biochemistry and Molecular & Cellular Biology at Georgetown University and corresponding author of the study. “That’s why our identification of Y5R’s involvement in initiating such genetic alterations is important, as it gives us a target to aim at or block that could avert cancer genome evolution and resulting progression to metastatic tumors that are resistant to chemotherapy.”
The current standard of care for Ewing sarcoma involves systemic cell-killing chemotherapy, which can affect all cells in the body, leading to side effects. There are no treatments targeted at genetic alterations that are used in routine treatment of Ewing sarcoma, which might make treatments less toxic. In particular, adequate treatments for patients with metastatic disease are lacking.
There are currently a number of drugs available that target Y5R because it’s also implicated in regulating food intake and psychiatric disorders. Several Y5R-targeted drugs have been successfully used in animal studies; one of them was used in human clinical trials for obesity. However, most of them are designed to block functions in the brain that inhibit food intake. According to Kitlinska, the main challenge will be to design Y5R-targeted drugs that do not cross the blood-brain barrier, as these effects are undesirable in cancer patients.
“We will keep performing experiments in mice in order to try to identify the mechanisms triggering spread of Ewing to the bone,” says Kitlinska. “Findings in Ewing sarcoma may also be relevant to other cancer types known to have high expression levels of Y5R, including another pediatric cancer, neuroblastoma, as well as common adulthood malignancies, such as breast, prostate and liver cancers.”
In addition to Kitlinska, the other authors from Georgetown include Congyi Lu, Akanksha Mahajan, Sung-Hyeok Hong, Susana Galli, Shiya Zhu, Jason U. Tilan, Nouran Abualsaud, Mina Adnani, Stacey Chung, Nada Elmansy, Jasmine Rodgers, Olga Rodriguez, Christopher Albanese, Hongkun Wang, Jan Blancato, G. Ian Gallicano, Michael Girgis, Amrita Cheema, Ewa Krawczyk and Luciane R. Cavalli; Maureen Regan is from the University of Illinois, Chicago; Valerie Zgonc and Svetlana D. Pack are from the National Cancer Institute; and Ewa Iżycka-Świeszewska is from the Medical University of Gdańsk, Poland.
Funding includes grants 1RO1CA123211, 1R03CA178809, R01CA197964, and 1R21CA198698 from the National Cancer Institute as well as grants from the Sunbeam Foundation and Children’s Cancer Foundation.
The authors report having no personal financial interests related to the study.