Understanding Immunotherapy Resistance Leads to New Therapeutic Strategies — and Hope
Posted in Lombardi Stories | Tagged cancer, cancer research, clinical trials, immunotherapy
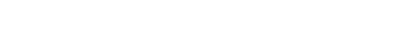
(January 18, 2024) — Samir Khleif, MD, remembers the eureka moment.
An experiment in his lab testing the effectiveness of immunotherapy in mice with cancer revealed some surprising results. All the mice had been given an immune-priming vaccine in addition to the immunotherapy, but only the mice that received the vaccine with or before the therapy improved; the ones that received therapy first stopped responding to treatment.
Khleif, who had been focused on getting the therapy to work, said he “flipped.”
“I realized we needed to look at why the immunotherapy wasn’t working, not why it was working,” said Khleif, an immunologist and professor of oncology at Georgetown University’s Lombardi Comprehensive Cancer Center.
Answering that question would lead him to a discovery that helps explain why some cancers become resistant to immunotherapy — and how that resistance can be overcome. Khleif’s findings form the basis of two clinical trials at Georgetown testing new ways of combining drugs to treat immunotherapy-resistant ovarian, lung and pancreatic cancers.
A Medical Breakthrough — With a Big Caveat

The discovery of immunotherapy was a medical breakthrough that led to new, highly effective therapeutic options for some cancers previously considered untreatable or with low survival chances. But despite all the progress that has been made, it still has a major limitation: It’s only effective in around 15% of patients with advanced cancer.
Some cancers are resistant to immunotherapy from the outset, while others may initially seem to improve with treatment, only to eventually stop responding.
Understanding why so many cancers are resistant to currently available immunotherapy — and developing strategies to overcome that resistance — are the goals that drive Khleif’s research.
“Over the past 30 years, we’ve improved immunotherapy tremendously, and the success rate has increased,” Khleif said. “However, our non-success rate is still staggering, and people are still dying of cancer.”
“To understand and, more importantly, to break through and see the other side of that, to develop strategies and solutions, and then to see an outcome that’s better than what is available, this is what I hope for,” he added.
Previous studies have tried boosting immunotherapies by combining them with other drugs and treatments. But when drugs were combined without fully understanding how they interacted with cancer and the immune system at the molecular level, they often failed. Thousands of clinical trials testing combination therapies failed to show clinical benefit, Khleif noted.
“We were the first to report that some immunotherapies could cancel each other out,” he said. “So understanding how immunotherapies work together is crucial to enhance their effect.”
He decided to take a closer look.
Priming T-Cells for Attack
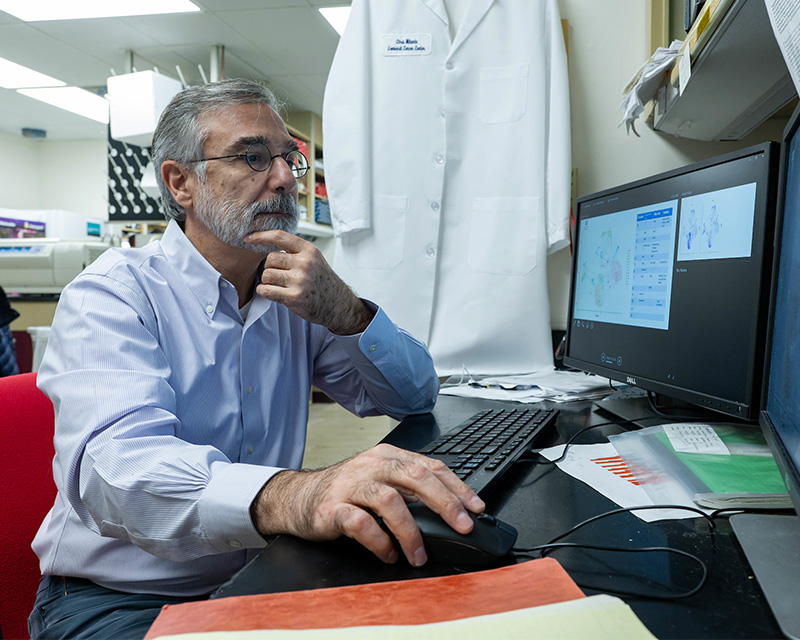
Khleif said he brings his experience as a physician to his research.
“Our work is to uncover fundamental biologic concepts in immunology, and when we’re doing science in the lab, I’m always thinking about how it could be applied to patients,” he said.
Khleif’s work has focused on understanding T-cells, a type of immune cell that fights cancer and other diseases. While cancer cells can evade the immune system by deactivating T-cells, checkpoint inhibitors, a common class of immunotherapy, work by disabling the “off” switch on T-cells, essentially unleashing them onto cancer in full attack mode.
Researchers have explored combining checkpoint inhibitors with a priming vaccine to activate T-cells. But when Khleif’s postdoctoral fellow showed him that the mice who received checkpoint inhibitors before the vaccine became resistant to the effective immunotherapy, he looked closely at what was happening. He found that these mice had high levels of a new type of T-cell that were dysfunctional and appeared to increase resistance.
“We found that if we give CPI alone without activation, these dysfunctional T-cells actually increase in number, and that becomes really bad for the success of immunotherapy,” he said. “Even if the immunotherapy works in the first round, if you start on the wrong foot, you will make that immunotherapy not effective anymore.”
He published his finding in 2019 in the journal Nature Immunology.
Forging a Unique Partnership

The new clinical trials build on these discoveries. In the first trial, patients with treatment-resistant ovarian cancer will be given the T-cell priming vaccine prior to a checkpoint inhibitor immunotherapy. The goal is to see if this strategy can overcome the cancer’s resistance.
“Ovarian cancer is just not responsive to immunotherapy from the outset, and that makes it very difficult to treat when it’s advanced and we’ve exhausted chemotherapy,” he said. “So it’s a real area of need.”
A second trial, for patients with advanced non-small cell lung cancer, as well as patients with pancreatic cancer, involves combining all three concepts. Patients will first be given a drug to deplete their dysfunctional T-cells, then a priming agent to activate their healthy T-cells, and finally, a checkpoint inhibitor immunotherapy.
To make this trial possible, researchers forged a unique collaboration with three different pharmaceutical companies: Janssen Pharmaceuticals, Bristol-Myers Squibb, and Targovax. Each company had one of the drugs needed for the proper treatment, but none had all three, Khleif noted.
“No one entity can do this,” he said. “That’s why it’s important for private companies to work together, and to join with an academic institution like Georgetown, because this is where this kind of research can happen.”
Both trials are currently enrolling patients.
After spending months or even years thinking about a scientific problem, Khleif said the “eureka moment” of discovery is thrilling. But ultimately, improving patient outcomes is what he finds most rewarding about his work.
“At the end of the day, my goal is to take a group of patients that did not have options before and provide them with a better quality of life and a longer life,” he said. “And just as importantly, the other goal is to make discoveries that other researchers can use as a springboard to do the same.”
This research was funded in part by the Department of Defense, AstraZeneca and Johnson & Johnson. Additional support was provided by the Georgia Cancer Center and Lombardi Comprehensive Cancer Center (P30 CA 051008).
Khleif is an inventor on a patent application related to technology described. Khleif reports the following disclosures: stock and/or ownership interest in Georgiamune, Precision Immunotherapy, Ayala (formerly Advaxis), IO Biotechnology, PDS Biotechnology, KAHR Medical, Sandbox Inc., and Northwest Biotherapeutics. Khleif is an advisor to Aligos Therapeutics, Aummune, Bayer Consumer Care, FREE Foundation for Research & Education Excellence, GI Innovation, Incyte, Nectin TX, Northwest Biotherapeutics, RAPA Therapeutics, Sandbox Inc., Stemline Therapeutics Inc. Khleif reports research contracts with AstraZeneca and Bristol-Myers Squibb.
Ilima Loomis
GUMC Communications