Investigational Drug Shows Promise in a Clinical Trial for Lung Cancers With ALK Mutations
Posted in News Release | Tagged cancer, clinical trials, gene sequencing, non-small cell lung cancer
For More Information
WASHINGTON (November 8, 2024) — The treatment landscape for non-small cell lung cancer (NSCLC) has progressed rapidly over the past decade, and now early signals from phase 1 of the ALKOVE-1 clinical trial suggest potential benefit from the use of an investigational drug called NVL-655 in people whose cancer has alterations in a gene called ALK. Patients are now being recruited for phase 2 of the trial at Georgetown University’s Lombardi Comprehensive Cancer Center and 53 other centers nationwide. Georgetown Lombardi is the research partner for the MedStar Georgetown Cancer Institute.
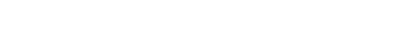
These findings would not have been possible without next-generation gene sequencing. The technique allows for the rapid analysis of DNA and the identification of rare genetic alterations in non-small cell lung cancer for which approved targeted therapies and novel agents, such as NVL-655, are utilized. This sequencing is part of the standard of care at Georgetown Lombardi and other cancer centers for all patients with newly diagnosed non-small cell lung cancer.
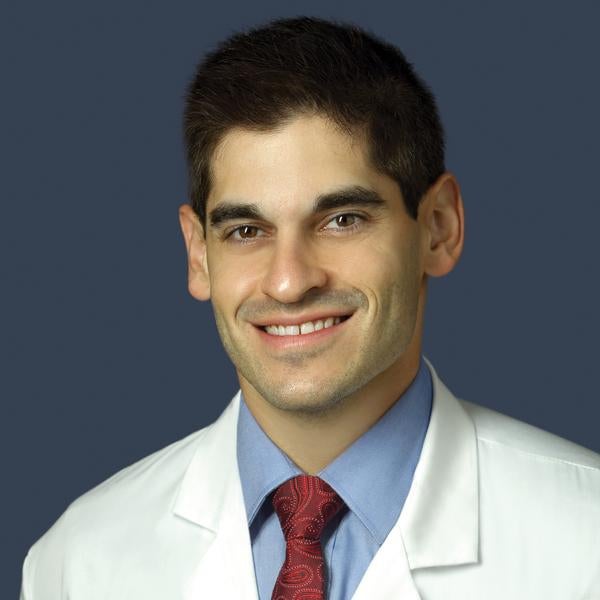
“Until about June of this year, most of us who saw patients with lung cancers that had ALK mutations used either alectinib or brigatinib, both second-generation targeted therapies, or a third-generation ALK inhibitor called lorlatinib, as an initial treatment option,” says ALKOVE-1 trial investigator Joshua Reuss, MD, assistant professor of medicine at Georgetown University School of Medicine and Georgetown Lombardi member. “Recent results from a major clinical trial called CROWN may be shifting more investigators to use lorlatinib as a first therapy, given the trial’s impressive findings of longer progression-free survival and increased activity against brain metastases compared to a first-line ALK inhibitor called crizotinib.”
While previous generations of ALK-targeted drugs have shown high response rates, resistance to the drugs has been inevitable. This prompted researchers to develop novel compounds to enhance efficacy and improve the side-effect profile of these drugs. NVL-655 is one such compound.
“We are building a better mousetrap, so to speak, to overcome the resistance mechanisms that we see as potential pitfalls with lorlatinib and other earlier generation targeted therapies,” says Reuss, who treats patients at MedStar Georgetown University Hospital.
Lorlatinib targets ALK fusion mutations that occur when the ALK gene joins with another gene to create an abnormal ALK protein that in turn causes cancer cells to grow and spread. But it also targets other mutations, including TRK, which may be responsible for some of the more relevant side effects that limit giving higher doses of the drug, as well as side effects that impact quality of life. NVL-655, however, is designed to specifically target only ALK mutations that develop due to resistance to other ALK-targeted drugs. Ultimately, the ALKOVE-1 trial will determine if NVL-655 can help improve efficacy while limiting side effects.
In September 2024, interim study results based on 103 patients assessed for efficacy in phase 1 of the ALKOVE-1 trial, which looked at safety and tolerability of the drug, were presented at the 2024 ESMO Congress in Barcelona, Spain. Treatment with NVL-655 at doses ranging from 15 mg to 150 mg once daily resulted in partial responses in over a third of evaluable patients and established that an optimal phase 2 dosage should be 150 mg daily. The preliminary objective response rate, which is the percentage of patients in the trial who experience a complete or partial response to treatment within a specific time period, was 35% in those who had already received two or more ALK-targeted drugs and 53% in those who had not received prior treatment with lorlatinib. Significantly, disease responses to the drug were seen in the brain, including patients whose disease had progressed on lorlatinib.
Physicians started recruiting patients for phase 2 of the trial in February 2024 and seek to determine, as a primary goal, the effectiveness of NVL-655 by assessing the response rate in up to 470 patients. They also hope to be able to assess how long the response lasts, how long it takes for a response to develop, how many people are still alive without their disease progressing after a certain period of time and, ultimately, how many people survive over a five-year or longer period of time.
About 70% of patients enrolled so far in the trial are non-smokers, and more than 50% of patients had a history of brain metastases. Most of the patients in the trial have been treated with multiple ALK-targeted medications prior to enrollment, as their earlier treatments were no longer effective. Patients with other rarer tumor types whose cancers may have an ALK fusion are also eligible to enroll in the trial.
“We encourage physicians who are treating NSCLC patients whose cancers have ALK mutations that are not responding to other drugs to consider enrolling their patients in ALKOVE-1,” says Reuss.
This clinical trial is supported by Nuvalent, which developed NVL-655. The ALKOVE-1 clinicaltrials.gov identifier is NCT05384626.
Reuss reports serving on the Advisory Board and/or as a consultant to these pharmaceutical companies: AstraZeneca, Bristol-Myers Squibb, Arcus, AbbVie, Daiichi Sankyo, Catalym, Seagen, Gilead, Janssen, Novocure, Regeneron, Summit Therapeutics and Pfizer.
Research funding to Georgetown for this study was supported, in part, by Genentech/Roche, Verastem, Nuvalent, the LUNGevity Foundation, Exelixis, Arcus and Revolution Medicine.