Case Study Reveals Important New Details About Rare Second Cancers Related to CAR-T Therapy
Posted in News Release | Tagged blood cancer, cancer, CAR-T therapy, multiple myeloma
Media Contact
Karen Teber
km463@georgetown.edu
WASHINGTON (June 12, 2024) — A new, detailed analysis of a patient’s second cancer after receiving CAR-T therapy for the initial cancer provides rare but important insights intended to offer helpful guidance for oncologists and pathologists about the clinical presentation and pathologic features involved in a CAR-T related second cancer.
The finding is reported June 13, 2024, in the New England Journal of Medicine.
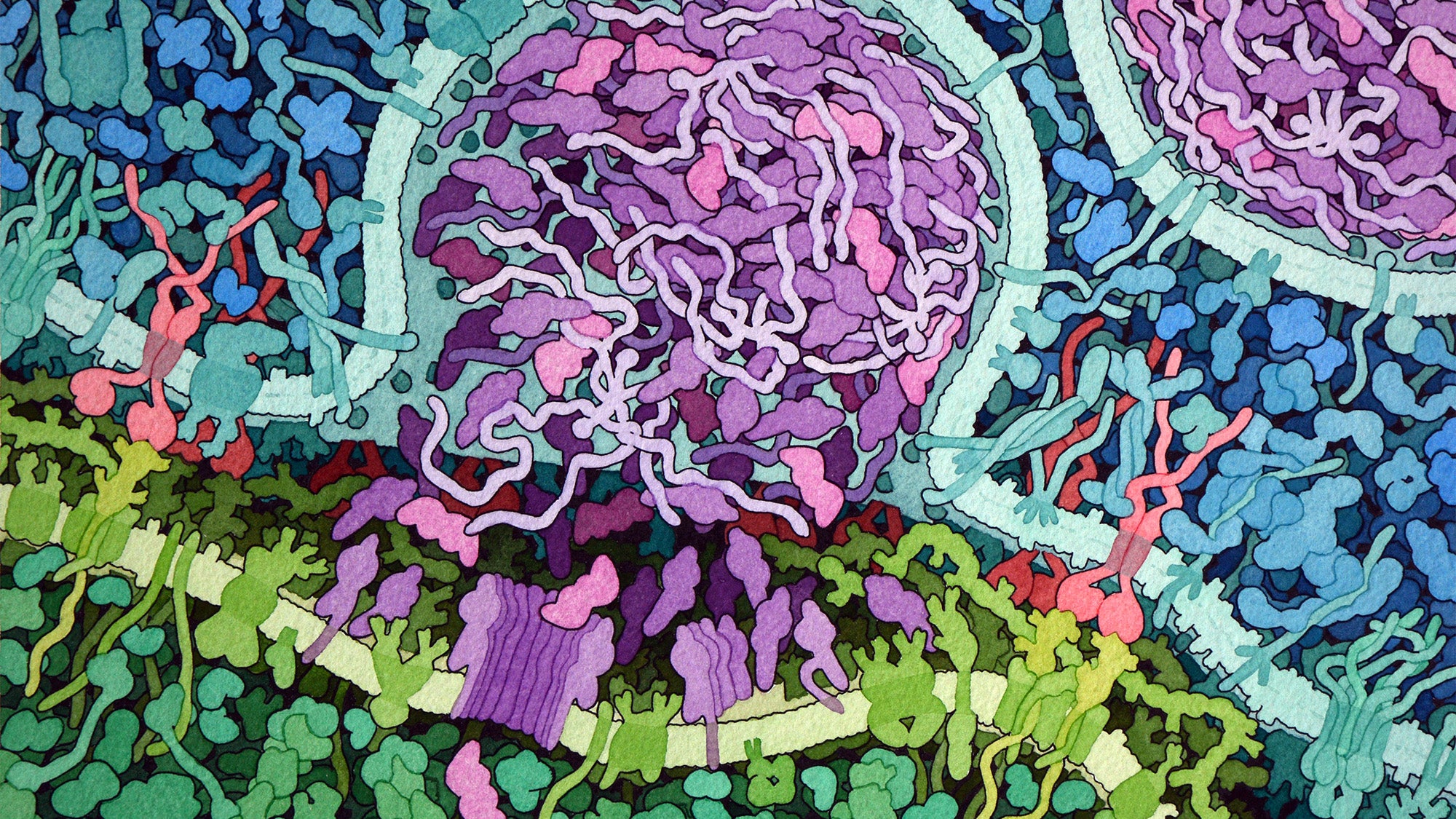
CAR-T therapy is described by many as a new and promising treatment for blood cancers. The therapy is made from a patient’s own cells, whereby immune system T cells are collected and re-engineered in the laboratory to produce proteins on their surface, called chimeric antigen receptors, or CARs. The CARs can recognize and then bind to specific proteins on the surface of cancer cells. The therapy is used to treat blood cancers such as multiple myeloma, the type of cancer the patient in the case study had when treated with CAR-T.
“The established value of CAR-T treatment and its benefits to cancer patients is significant,” says the study’s first author, Metin Ozdemirli, MD, PhD, professor of pathology at Georgetown University School of Medicine and attending physician and director of the Hematopathology and Hematology Laboratories at MedStar Georgetown University Hospital. “Our case study describes a rare event in a patient who received CAR-T therapy and provides very useful information for physicians treating patients with this approach. Armed with our insights, physicians can be on the lookout for similar conditions and potentially detect secondary tumors earlier and manage them better.”
Of the estimated 30,000 patients treated with CAR-T therapy, reported second cancers are rare; the U.S. FDA has tracked approximately 25 cases of CAR-T cell second cancers, usually lymphomas, as occurred in the patient in this case study following CAR-T cell therapy.
How the CAR-T cell became a lymphoma is not known. It is possible that the cells had lymphoma-causing mutations when they were originally collected from the patient and CAR-T treatment caused activation and expansion of those cells; or the mutations might have occurred when the CAR-T cells were prepared outside the patient; or the CAR-T cells may have acquired the mutations after they were given back to the patient; or any combination of these circumstances.
Four months after receiving CAR-T therapy, the patient in the case study developed progressively worsening non-bloody diarrhea and lost 12 pounds. Results of bloods tests led to an endoscopic exam revealing ulcerations in the duodenum, the first part of the small intestine. The patient received treatment, but symptoms persisted, resembling an autoimmune disease. After numerous additional tests, biopsies taken revealed the culprit — indolent T-cell lymphoma of the gastrointestinal tract, similar to other cases, but further molecular analysis showed this to be a CAR-T positive case.
Ozdemirli says this case study suggests that physicians treating patients with CAR-T should always consider CAR-T a potential source for new cancers and autoimmune problems. “When we know what to look for ahead of time, it becomes easier to catch problems earlier,” he says.
Ozdemirli also points out, “An interesting finding here is the type of cells that survived the initial treatment and became cancerous. Immune cells that are collected from patients to prepare the CAR-T cocktail are not a homogenous single-cell type. They contain a mixture of multiple cells, and in the case of this patient, what is called a helper T cell, an essential infection-fighting cell, unexpectedly was the culprit.”
Though uncommon, second cancers following chemotherapy or radiation therapy can develop. Just like any tissue in the body has the risk of developing cancer during a lifespan, CAR-T cells carry the same risk. Ozdemirli says so far there is no evidence to suggest that the process of preparing the CAR-T population outside the body increases that risk.
Importantly for diagnostic and treatment purposes in the future, the researchers note that switchable cell therapies might allow patients to take a medication to tune the amount of CAR-T cell activity from day to day, hopefully reducing toxic side effects. Advancing this research and knowledge is an important next step for the investigators.
In addition to Ozdemirli, the co-authors include Thomas M. Loughney, MD, Emre Deniz, PhD, Joeffrey J. Chahine, PhD and Aykut Üren, MD, at Georgetown University; Maher Albitar, MD, Genomic Testing Cooperative, Irvine, California; Stefania Pittaluga, MD, NIH, Bethesda, Maryland; Sam Sadigh, MD, Brigham and Women’s Hospital, Boston; and Philippe Armand, MD, PhD, and Kenneth C. Anderson, MD, Dana-Farber Cancer Institute, Harvard Medical School, Boston.
This work received no external funding.
Disclosures provided by the authors are available with the full text of this article at NEJM.org. Dr. Ozdemirli has nothing to disclose.
