Analyzing Tumors in Real Time to Detect Metastatic Cells Could Aid in Treatment
Posted in Lombardi Stories | Tagged cancer, interdisciplinary research, metastasis risk
(November 12, 2020) — Identifying cells that metastasize from the primary tumor to other sites in the body, thereby expanding their lethality, has been a goal of scientists for years. If researchers knew more about what gives metastatic cells their ability to spread and grow throughout the body, there would be a better chance to detect and eradicate them before they cause extensive harm.
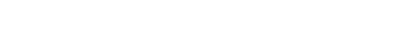
(image taken prior to COVID-19 pandemic)
That’s why a collaborative, cross-institutional team of cancer biologists and physicists at Georgetown University and Georgetown Lombardi Comprehensive Cancer Center have been collaborating on a device that could advance this goal.
“There’s a marathon being run in a tumor, and the winners, from the tumor’s perspective, are the cells that can quickly escape the tumor’s locality and spread to other sites, boosting their longevity,” says Anton Wellstein, MD, PhD, professor of oncology and pharmacology at Georgetown Lombardi. “The tool we developed allows us to isolate the marathon ‘winners’ and study those cells to determine what makes them unique and especially nasty.”
“Usually the cells in a tumor that become metastatic are a very small percentage,” explains Ghada Sharif, PhD, research assistant professor in Wellstein’s lab at the cancer center. “The problem has been, how to tell which cells in a tumor have metastatic potential. For that we turned to our colleagues in the physics department at Georgetown University to help us devise a system to isolate metastatic cells from others.”

(image taken prior to COVID-19 pandemic)
The device they built, with the support of a collaborative grant from Agilent Technologies, Inc., is a modification of the company’s xCELLigence device. The modified instrument allows mixtures of cells extracted from tumor biopsies, placed in a top chamber, to pass through a porous membrane. Because of their aggressive nature, the metastatic cells pass through the membrane first, allowing for isolation and collection.
“The commercial device we acquired had two chambers; we modified the second chamber and added a third, all of which allowed us to easily separate out and collect the cells we were most interested in, which were the metastatic cells,” says Makarand (Mak) Paranjape, PhD, associate professor in physics and director of Georgetown’s Nanoscience and Microtechnology Lab.
“It took an iterative process over a year’s time to converge on our final system implementation, and we now have a patent pending for our device,” says Paranjape. “I believe it holds the potential to be a significant diagnostic tool for clinicians to use in identifying early signs of metastasis risk and give physicians the ability to target and eradicate the cells early in the course of the disease.”

(image taken prior to COVID-19 pandemic)
He also noted that none of these modifications would have been possible without the ingenuity of Georgetown physics department machinist Leon Der.
Another significant benefit of the modified device is its ability to co-culture cells from either the tissue surrounding tumors or immune cells and place them in a separate chamber from the tumor cells. These cells provide chemical signals, or cues, to metastatic cells that may affect their mobility. According to Sharif, they’ve looked at about seven different types of cancer cells so far, including those originating in the breast and pancreas, and regardless of the type of cancer cell, the ability to isolate the metastatic cells from other cells remained reliable.
Now that the research in the lab has proved fruitful, the scientists are grafting human cancer tissue to mice to watch how cancer cells metastasize in the animals. They are then able to study the metastatic ability of those tumors when the tissue is placed in their new device. If the animal experiments are productive, the researchers hope to test their device in the clinic over the coming years.
“The key question is whether information gathered from our device can aid in making decisions about how to treat a patient,” concludes Wellstein. “One of the hardest questions in cancer is trying to understand how the heterogeneity of a tumor, particularly where only a small number of cells metastasize, impacts a patient’s outcome. With perseverance, we hope to provide a way to answer that question in the near future.”
Disclosure: Georgetown University owns intellectual property directed to this research with Wellstein, Der, Sharif and Paranjape as named inventors on the patent application.
Michael Miller
GUMC Communications