Georgetown Global Health and Cancer Researchers Tackle Public Health Challenge in Eswatini

Posted in Lombardi Stories | Tagged cervical cancer, Eswatini, global oncology, HIV, HPV
(June 20, 2024) — A collaboration between researchers at Georgetown’s cancer center and a Georgetown global health team in Eswatini aims to address a significant public health challenge: preventing cervical cancer.

Cervical cancer remains a leading cause of suffering and death among women globally, despite being preventable through vaccination and treatable if detected early. In 2020, there were approximately 604,000 new cervical cancer cases and 342,000 deaths worldwide, making it the fourth most frequently diagnosed cancer among women.
The burden is disproportionately high in low- and middle-income countries, particularly in sub-Saharan Africa. In Eswatini, with one of the highest HIV prevalence rates globally, the dual burden of HIV and cervical cancer necessitates integrated and robust health care interventions. Current guidelines recommend annual screening for HIV-positive women and less frequent screenings for HIV-negative women.
Game-changing Cervical Cancer Screening
To better target interventions, and improve cervical cancer screening and care for women living with HIV in Eswatini, researchers from Georgetown’s Center for Global Health Practice and Impact (CGHPI) teamed up with screening experts from Georgetown’s Lombardi Comprehensive Cancer Center and the University of New Mexico.
The team analyzed clinical records from women aged 15 and older who accessed visual inspection with acetic acid (VIA) cervical cancer screening from health facilities in the Lubombo and Manzini regions of Eswatini between October 2020 and June 2023.
VIA is a simple and inexpensive cervical cancer screening test where acetic acid (often associated with vinegar) is applied to the cervix. White spots on the cervix can indicate the presence of abnormal cells that can be treated, potentially preventing a progression to cancer. Additional screening is recommended.
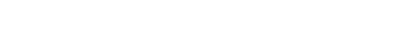
“VIA is a game changer, as it picks up potential cancer early, before progression and symptoms, which enables people to be treated at a precancerous stage with better treatment outcomes,” said Christopher Loffredo, PhD, director of Georgetown Lombardi’s Office for Global Oncology and co-leader of the study.
Meeting WHO Screening Standards
Information from this study could help usher in changes to cervical cancer screening, Loffredo said. While VIA is a “standard of care” test for women, Eswatini recently adopted the use of human papillomavirus (HPV) DNA testing in accordance with World Health Organization guidelines.

“The HPV DNA test identifies women who have the cervical cancer-causing strains of the virus and prioritizes them for surveillance and follow-up screening and care,” said Victor Williams, MD, CGHPI associate director for implementation and data science in Eswatini. “However, it will take some time and resources before this type of testing is available across the country. Until then, most women will continue to rely on VIA.”
In their study, Williams and his colleagues found that of 23,657 participants who underwent a VIA, 2.6% tested positive. Women screened at mission-owned, NGO-owned, and industrial/workplace-owned health facilities showed significantly higher odds of a positive VIA compared to those screened at government-owned facilities.
Loffredo said the difference in screening outcomes by type of facilities could be related to expertise.
“Most governmental health facilities have rotations of nurses through different clinical departments, which is not the same as NGOs, where experienced nurses are stationed for longer time periods, which allows them to build up their skills and experience,” Loffredo said.
Women aged 35-44 had a 1.26 times higher likelihood of a positive VIA compared to those aged 25-34. Key to their findings was that women on antiretroviral therapy (ART) for 5-9 years or ≥10 years, as well as having an undetectable viral load, significantly reduced the odds of a positive VIA screen.
The team published their results this spring in PLOS Global Public Health.
Next Steps
“There are many published reports that show the reduction of cervical cancer mortality by implementing VIA screening,” Loffredo said.
“We conducted this study to help us understand more about factors that are common among those who test positive for a VIA screening test and to understand what might be hindering women from getting tested,” said Williams.
The next step in their work is to apply for grants to scale-up the availability of HPV screening.
“We believe screening can have a positive impact in the lives of women in Eswatini,” Loffredo said. “A key component of success is to tailor the intervention to the population.”
Loffredo, along with the CGHPI’s Sharon Kibwana, MD, MPH, and Martine Etienne-Mesubi, DrPH, MPH, have met with stakeholders in Eswatini to plan for implementation science grant proposals.
“Implementation science starts with the premise that there are existing, evidence-based interventions to bring to bear on the problem of cancer prevention, and this is particularly true for cervical cancer screening in high-risk women living with HIV,” Loffredo said.
He added, “This kind of approach and the lessons we learn would be immediately relevant to neighboring countries in southern Africa that are facing the same dire consequences of HIV and cervical cancer.”